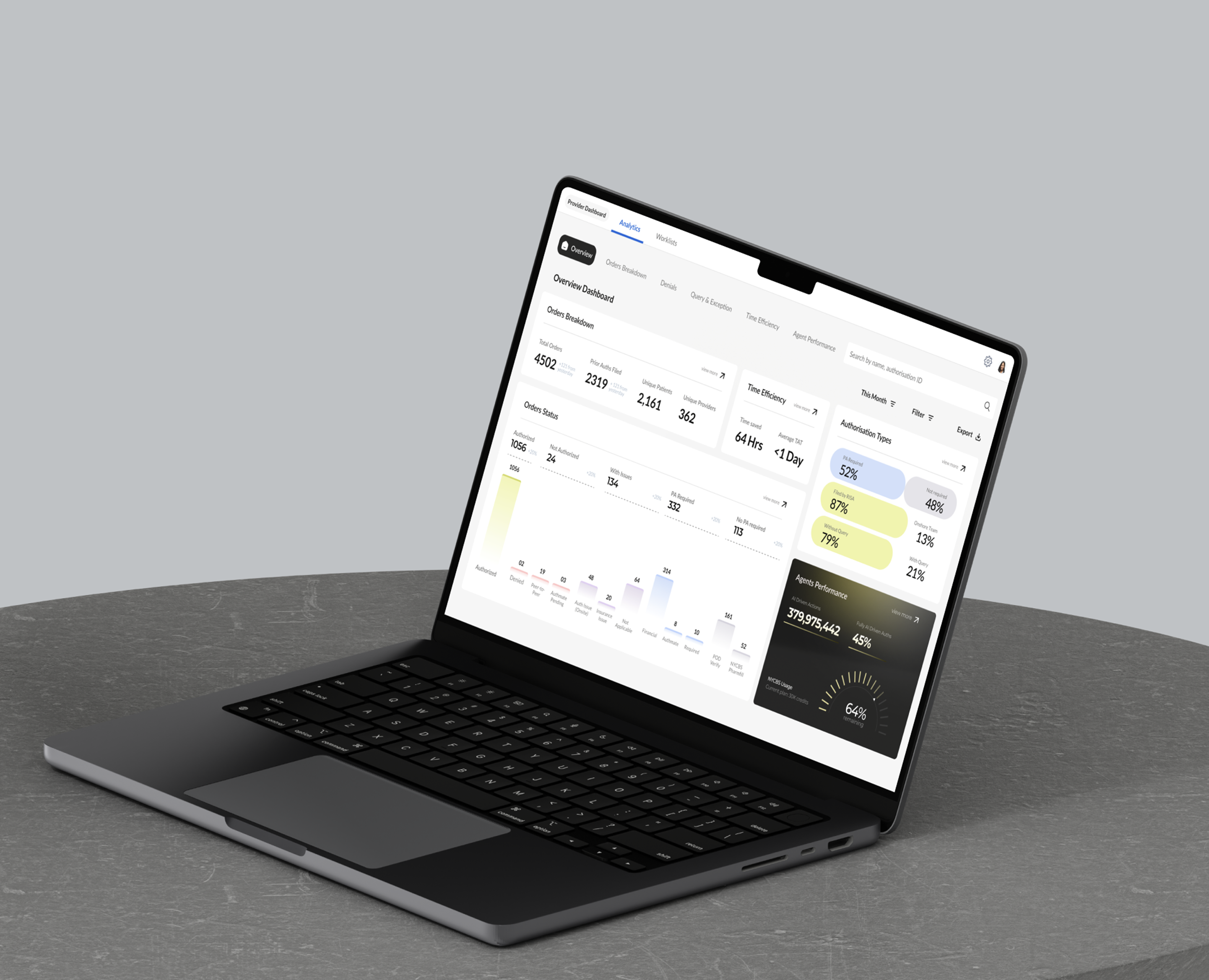
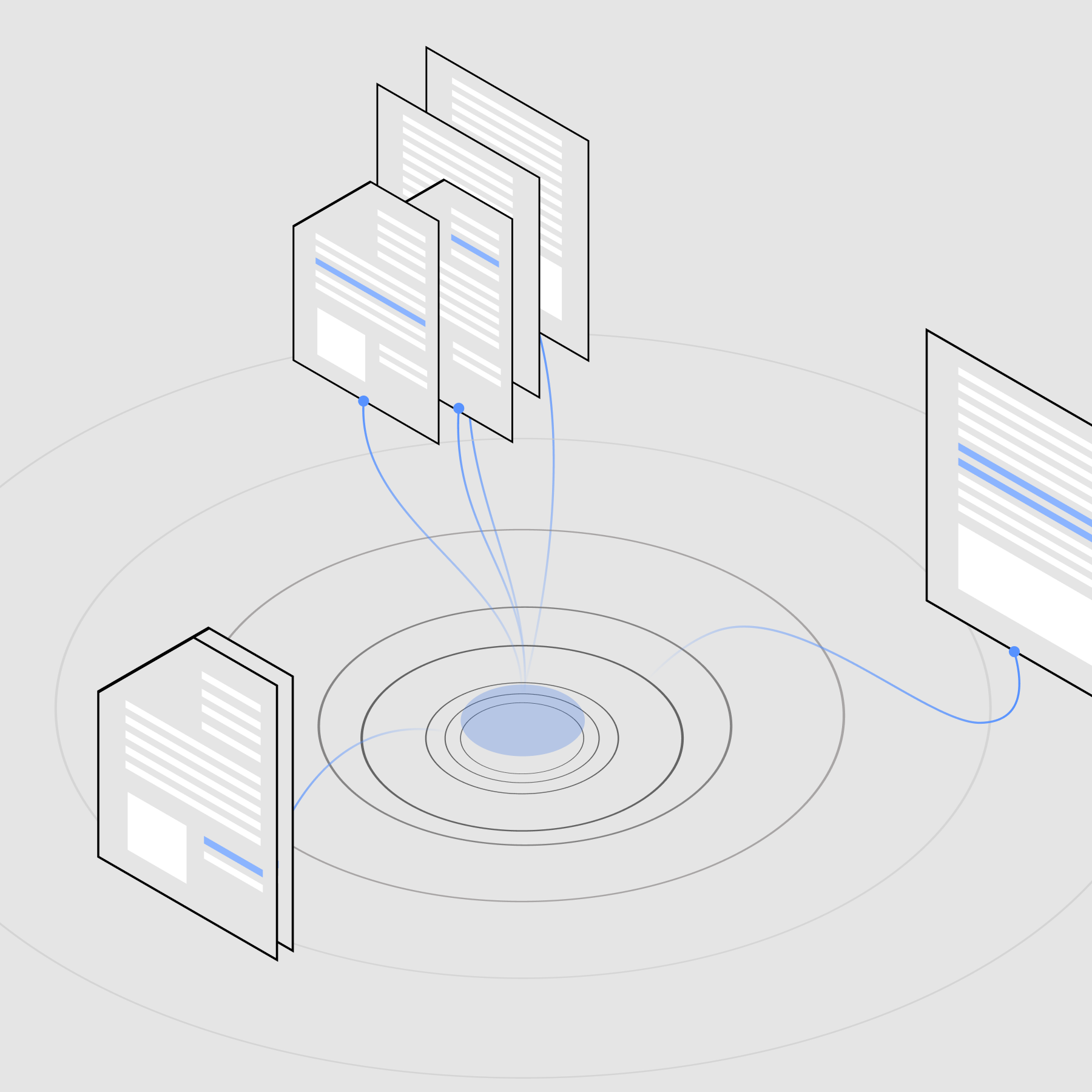
Part B + Part D Prior Authorization
End-to-end authorization execution for oncology drugs, resolving medical necessity, payer criteria, and submission across portals, APIs, and e-fax
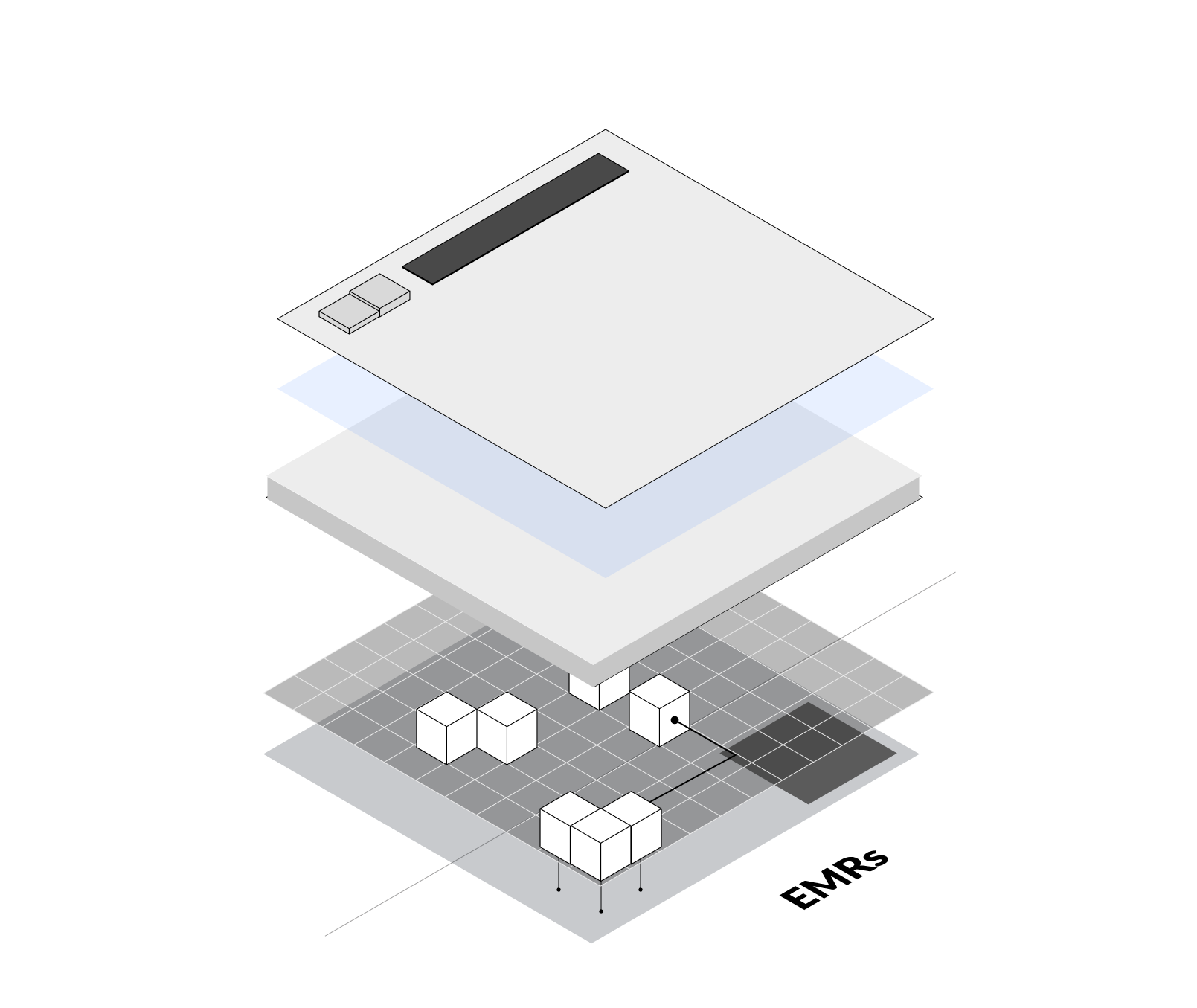
Eligibility & Benefit Verification
Real-time verification of coverage, benefits, and patient responsibility across payers, written back into the EHR
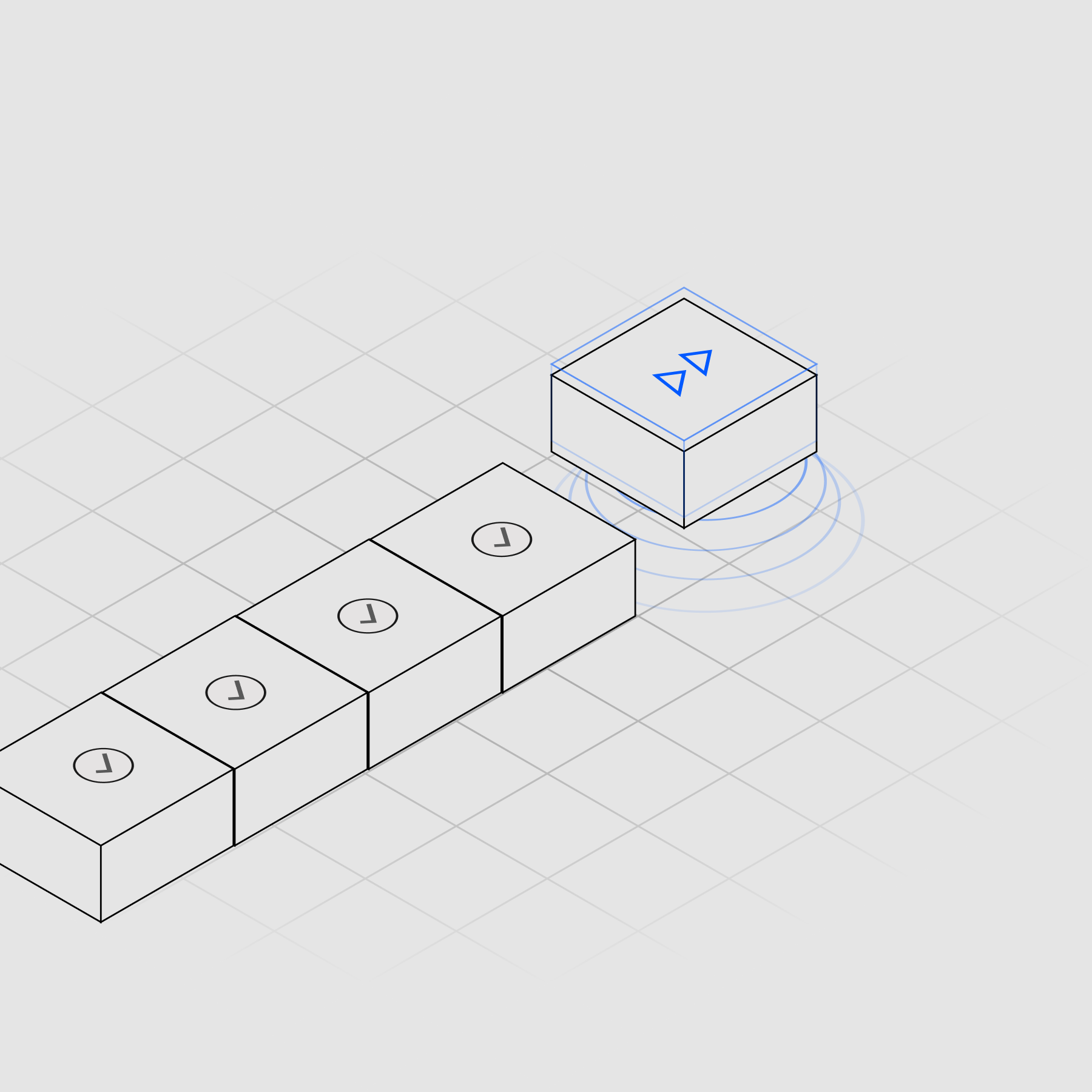
Claims Status
Automated claim status tracking with continuous reconciliation against authorizations, payer responses, and payment events
Denial Management
Systematic detection, classification, and resolution of denials with guideline-aligned appeals, evidence reuse, and closed-loop status updates
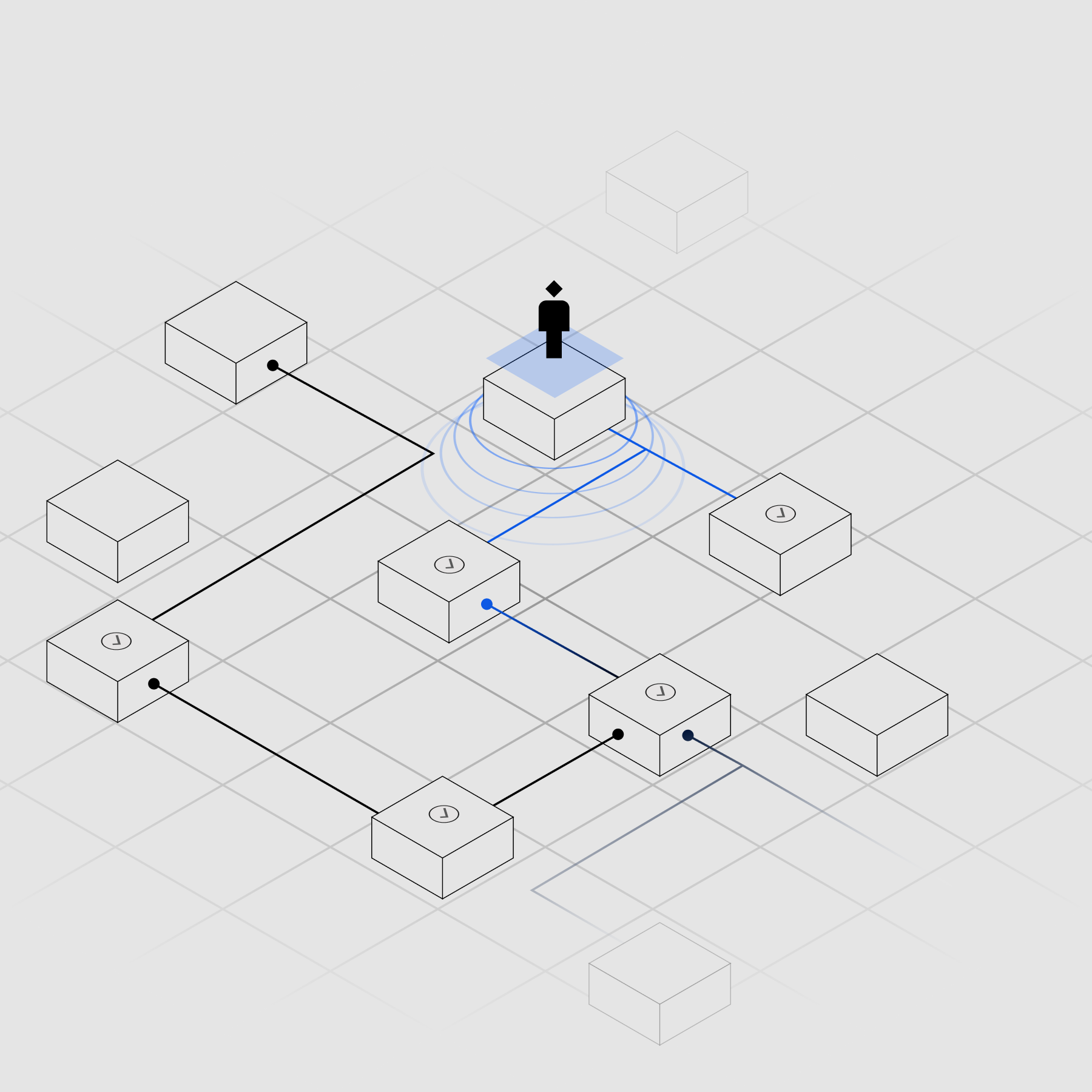
Clinical Decision Support
Continuous data capture across facilities without on-site personnel
Custom Workflows +
Composable, rules-driven workflows tailored to each practice’s SOPs, payer mix, and operational constraints




.png)

%202.png)

%201.png)